What is PBC?
Primary biliary cholangitis (PBC) is a rare disease, so it may be hard to find helpful information about it. Use this overview as a starting point and talk to your healthcare provider about your questions.
PBC is a rare autoimmune disease of the liver
PBC is chronic, meaning long-lasting, and progressive, meaning it can become worse over time.

PBC causes inflammation in the bile ducts of the liver

Over time, scarring from this inflammation can block the bile ducts, leading to liver damage and reduced liver function

If left untreated or not treated well enough, PBC can lead to end-stage liver disease and the need for a liver transplant
Diagnosing PBC
Diagnosing PBC early is important so you can take steps to try to prevent further liver damage as PBC progresses.
Healthcare providers can typically diagnose PBC using:
- Blood tests to measure abnormal amounts of certain substances in your blood that are caused by PBC
- FibroScans or biopsy (less common) to uncover evidence of liver scarring caused by PBC
What causes PBC?

Measuring PBC progression
Your healthcare provider may monitor a few things to see if your PBC is under control or progressing, including:
ALP
An enzyme also known as alkaline phosphatase or “alk phos.”
Scarring
FibroScans are used to measure the amount of scarring in your liver.

Research has shown that long-term elevated ALP levels are associated with liver damage that may ultimately require a liver transplant
PBC symptoms
When the liver doesn’t function properly due to PBC, it can lead to symptoms that you may not realize are caused by liver disease. Some of the most common PBC symptoms include:



Up to 80% of people with PBC experience itch. For some people, itch can even interrupt sleep, which may contribute to daytime sleepiness and fatigue
Talking to your healthcare team about your symptoms
It’s important to make sure your healthcare team knows about any symptoms you’re experiencing, including itch. They may be able to adjust your treatment plan to try to manage your symptoms.
Since itch can come and go, even if you aren’t experiencing itch during your appointment, it’s important to share how itch affects your day-to-day life.
Measuring itch with the Numerical Rating Scale (NRS)
The NRS is a scale from 0 to 10 that is used in clinical trials to track itch severity and progress. You can use the NRS to measure your itch over time and share the results with your healthcare team.


Working with a specialist
When you’re first diagnosed with PBC, your healthcare provider may refer you to a specialist.
- Hepatologists are doctors who specialize in treating the liver
- Gastroenterologists are doctors who specialize in treating the organs in your digestive tract, including the liver
These specialists have experience treating liver diseases and may have treated other people living with PBC. As such, these doctors should be more aware of the latest PBC treatment options and should be able to offer well-informed PBC management advice.
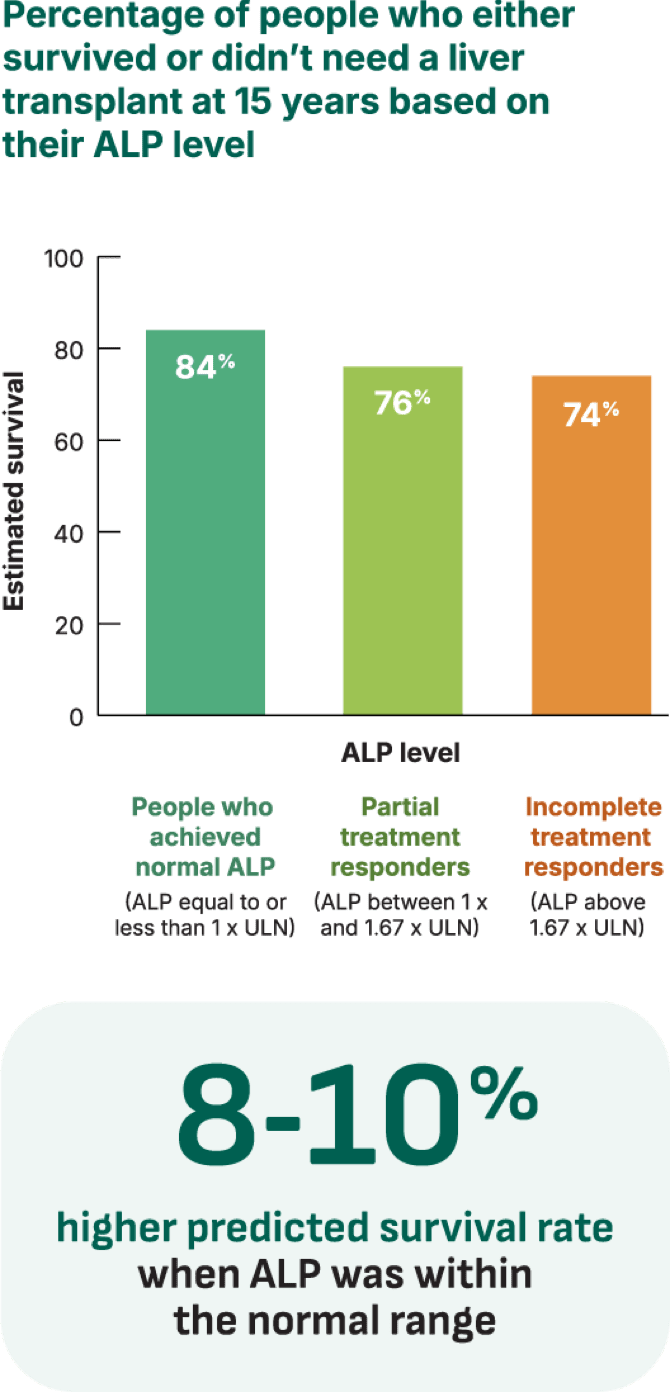
Your risk of PBC progression is reduced when ALP is normal or close to normal
Studies show that people with ALP levels consistently above normal have a higher risk of liver damage and transplant than those levels closer to normal.
Getting your ALP closer to a normal range, or at normal for longer periods, may help delay liver damage.
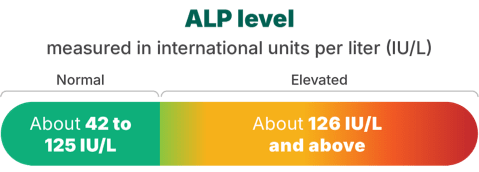
Everyone’s normal ALP range is different, but some labs suggest a normal ALP range is around 42 to 125 IU/L (international units per liter). Ask your liver specialist if your ALP is in the normal range.
The closer ALP was to normal, the higher the estimated survival (survival means people lived or did not need a liver transplant)
In one PBC study of data across 15 years, normal total bilirubin and ALP levels were used to predict the rate of survival for people living with PBC.
Survival estimates were calculated using the number of people who passed after liver transplant or for any other reason—this was the main measurement of the study.
Medical charts were collected from 17 centers across Europe and North America, and researchers studied follow-up data from 3,059 people to estimate how long a person may live with PBC based on normal total bilirubin and ALP level. The study included people treated with ursodiol and people who were untreated. Survival estimates included 2,005 people who were treated with ursodiol and reached a normal total bilirubin at 1 year.
ULN=upper limit of normal.
Is normal ALP possible?
ALP levels that are consistently above the normal range have been shown to cause permanent liver damage. That’s why lowering ALP levels to a normal range (your healthcare team might call this “normalizing ALP”) is one of the main goals of PBC treatment.
See how one PBC treatment did at normalizing ALP in a clinical trial.